Mental health is good medicine. That’s a mantra of Houston VA Medical Center and it’s putting mental health providers throughout the hospital—making it easier than ever to receive these services.
“Wherever we have patients, we want to meet them in that setting, providing integrated care working side-by-side with medical providers,” said Dr. Candy Smith, director of Behavioral Health Services.
Behavioral health takes a holistic approach with the Veterans it serves. A team of psychologists focuses on treating the interaction between the physical and mental health conditions.
“The functional limitations associated with some chronic illnesses and medical conditions can affect people’s moods and cause issues with anxiety,” said Dr. Frances Deavers, Houston VAMC psychologist attached to Cardiology Service. “For example, the link between depression and cardiac conditions is well researched.”
Patients who have suffered a heart attack are at a higher risk for depression. And patients who are depressed and have had a heart attack are at a greater risk to have another heart attack than someone who has had a heart attack but is not depressed.
“If patients are depressed or anxious, they can have problems making lifestyle changes that are necessary to optimally manage their medical conditions…ultimately leading to worse outcomes down the line,” Deavers said.
Behavioral health clinicians are in Primary Care, Gastroenterology, Infectious Disease, Palliative Care, Pain Clinic, Women’s Health Clinic, Post Deployment, Oncology, Organ Transplant, Sleep Clinic, Neuropsychology Specialty, and Cardiology Service. Veterans are reaping the benefits of these services every day.
Navy Veteran David Lee said, “I was happy to see how well staffed it was and how people were taking advantage of it. I was seeking counseling for depression and just happened to be a cardiology patient at the same time. I received good counseling and other methodologies for my problem, so it was a rewarding experience. I think it was serendipitous.”
Some Veterans are surprised to find a psychologist available in a clinical setting. “If a Veteran doesn’t understand how things fit together and how their mental and physical health conditions interact, maybe they are taken aback,” said Deavers. “I’m coming in for my heart, why am I seeing a psychologist?”
Patients are seeing a psychologist for two reasons. First, there is the mental to physical health correlation. If the Veteran feels good and positive mentally, there is a better chance his physical health will follow suit. If the patient is overwhelmed with crushing anxiety over the thought of having a pacemaker put in or going through an organ transplant, that is not an ideal environment for good health and well-being. And secondly, because some patients can be apprehensive about going to the sixth floor for mental health services. Bringing the psychologist to them in a clinical setting helps eliminate that issue.
“Our Veterans know that the sixth floor of our VA medical center is dedicated to mental health services and some of them may feel uncomfortable going there,” said Smith. “I’ve seen Veterans who are hesitant to press the button in the elevator for the sixth floor because they feel there is a stigma attached. Being able to see Veterans where they feel the most comfortable is important. We want to increase access to behavioral health/mental health services for those who may be hesitant.”
Family members also are welcome to participate in sessions between the therapist and patient. It can be beneficial to get the family member’s perspective and allow them to get an understanding of the condition and what’s going on for the Veteran.
“Sometimes the family members may need some caregiver support because they are doing a lot to make the house run and help the Vet get to appointments and manage things,” said Deavers. “I always welcome having family members participate in care if that is what the Veteran wants. I think it can be great, especially if we are working on adherence (the degree to which a patient correctly follows medical advice).”
Behavioral health services in these clinics are an option for Veterans. There is no pressure to see a psychologist, but the service is there if it’s needed.
“We plant the seed that we are available,” said Smith. “Maybe they don’t need us now, but they could need us later. Education is important, and we try to help providers discuss behavioral health services with their patients so it’s inviting and people can understand the benefits.”
“Because so many of the problems we (Veterans) have are psychological, it’s nice to see these services readily available,” said Lee. “It’s right there.”
Todd Goodman is a public affairs specialist at the Michael E. DeBakey VA Medical Center
Topics in this story
More Stories
Health summit gave Veterans opportunities to visit with VA staff and meet community organizations that provide services to Veterans.
STAR is a rehabilitation program for Special Operations Forces service members and Veterans. It facilitates recovery, function, reintegration, and transition.
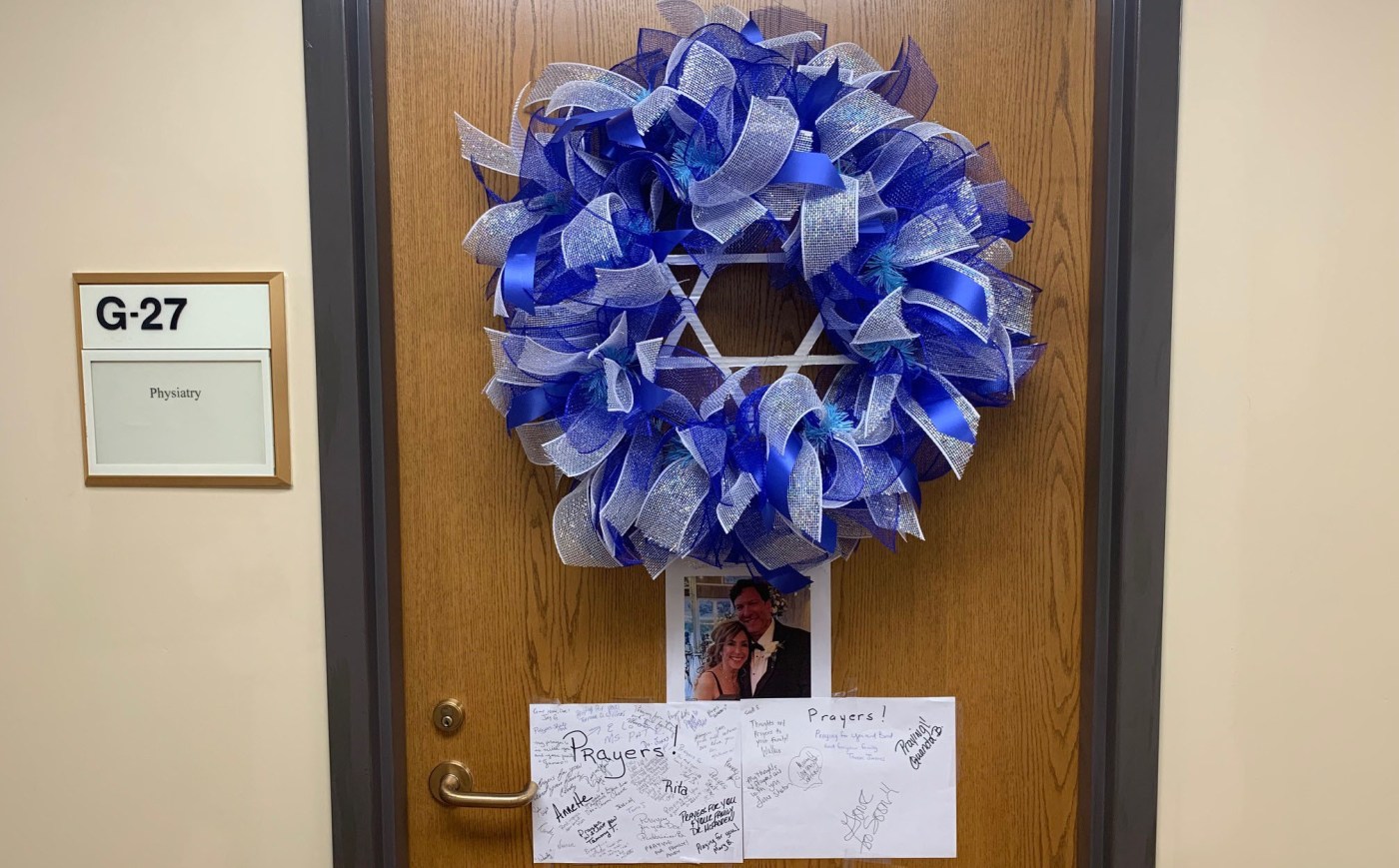
Dr. Cohen left his mark on the specialty care clinic staff and on the Tuscaloosa VA Medical Center as a whole.






I think this approach is helpful for patients who are apprehensive about seeking mental health services.
I believe this model is also helpful to the whole Veteran approach. So many mental and physical health conditions are concurrent; having this as an option will help so many more Veterans.
Go Houston VA.
The VA does its best. It could be a lot better.