As part of the U.S. Department of Veterans Affairs’ (VA) efforts to provide the best mental health care access possible, VA is reminding Veterans that it offers all Veterans same-day access to emergency mental health care at any VA health care facility across the country.
“Providing same-day 24/7 access to mental health crisis intervention and support for Veterans, service members and their families is our top clinical priority,” said VA Secretary Robert Wilkie. “It’s important that all Veterans, their family and friends know that help is easily available.”
VA’s Office of Mental Health and Suicide Prevention is the national leader in making high-quality mental health care and suicide prevention resources available to Veterans through a full spectrum of outpatient, inpatient and telemental health services.
Additionally, VA has developed the National Strategy for Preventing Veteran Suicide, which reflects the department’s vision for a coordinated effort to prevent suicide among all service members and Veterans. This strategy maintains VA’s focus on high-risk individuals in health care settings, while also adopting a broad public health approach to suicide prevention.
VA has supported numerous Veterans and has the capacity to assist more. In fiscal year (FY) 2018, 1.7 million Veterans received Veterans Health Administration (VHA) mental health services. These patients received more than 84,000 psychiatric hospital stays, about 41,700 residential stays and more than 21 million outpatient encounters.
Nationally, in the first quarter of FY 2019, 90% of new patients completed an appointment in a mental health clinic within 30 days of scheduling an appointment, and 96.8% of established patients completed a mental health appointment within 30 days of the day they requested. For FY 2018, 48% of initial, in-person Primary Care — Mental Health Integration (PC-MHI) encounters were on the same day as the patient’s PC encounter. During the first quarter of FY 2019, 51% of initial, in-person PC-MHI encounters were on the same day as the patient’s PC encounter.
Veterans in crisis – or those concerned about one – should call the Veterans Crisis Line at 800-273-8255 and press 1, send a text message to 838255 or chat online at VeteransCrisisLine.net.
Topics in this story
More Stories
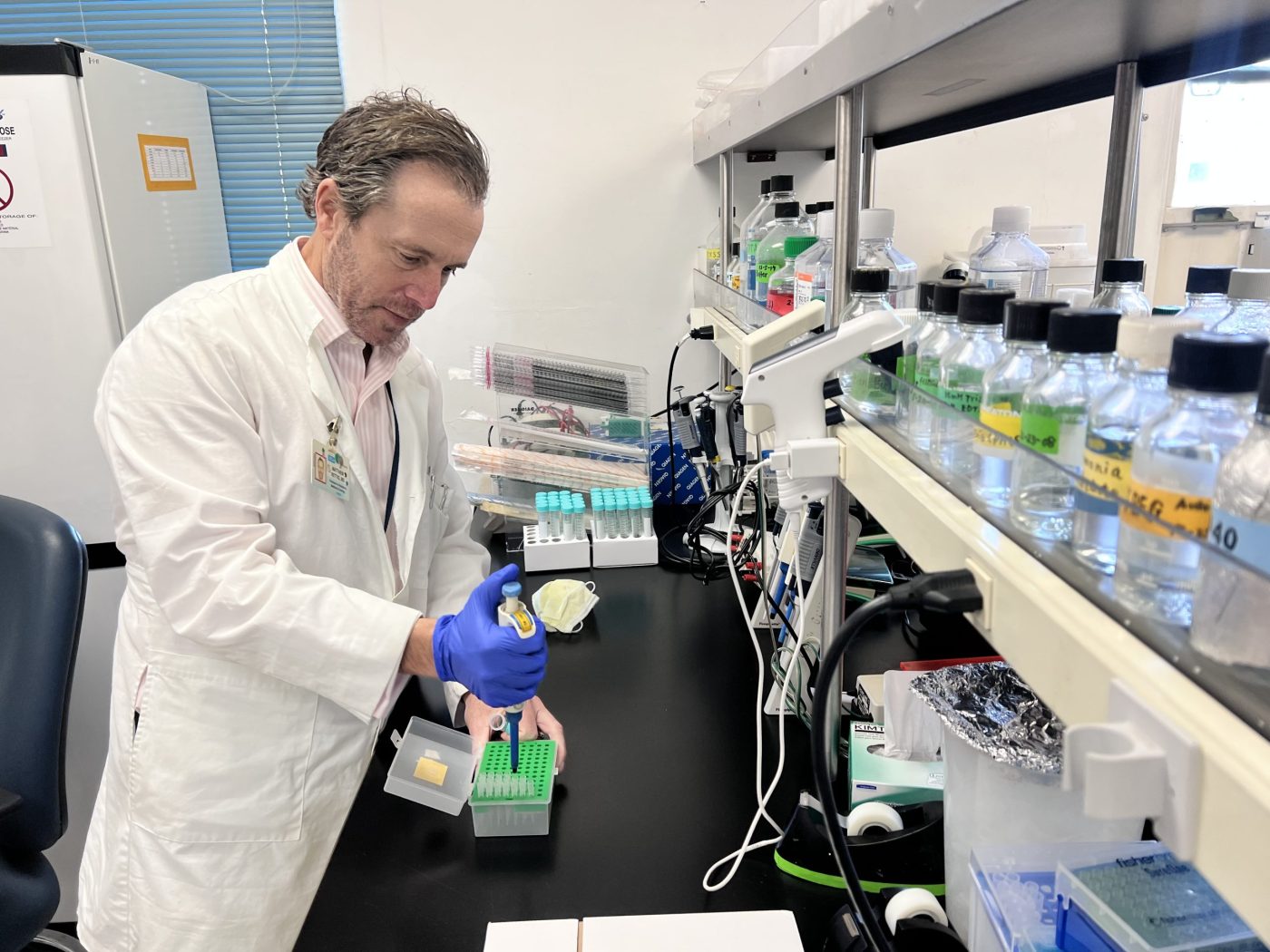
As part of a new research study that began July […]
WASHINGTON ― The Department of Veterans Affairs Office of Research […]
On Thursday, VA announced an updated version of its 1959 mission statement.





The OKCVAMC is punishing veterans for filing complaints. They are trying to lock them up and use dhs to take their children when doctors use the system against veterans instead of helping. They don’t read records and help they use the system to not help. This facility has a history of problems and they are very real right now.
I live in Utah and for me to get to the closest VA facility to be able to get the free 24/7 mental health access that the va says they offer I would have to travel 2+ hours to get that help. I would like to know how this helps those of us that are out of range of a va facility if we were in the event of needing this help can go to without having to wait to make an appointment or worse end our existence as has been very prominent lately. I am asking that the va look at this and set up local MH facilities that are within under an hours travel to battle the suicide rates of veterans. I know that the va says they don’t have a financial issue, so if this is the case then make these facilities closer and more accessible to those of us that live so far out from these facilities.
Why is it that when I called the Joplin, MO VA at 4:18 pm today April 29, 2019 there was no answer and the automated system said they closed at 4:30 pm, even when I put in the extension for mental health clinic. I’m going to have to call BS on the statements in this blog. Oh also I’ve been waiting since March 22, 2019 to be scheduled an appointment with a new provider. I was told first that Salt Lake City would be calling to schedule an appoint for video telehelath, waited several weeks never received a call, then when I called Joplin was told that the provider was already booked and they didn’t have enough providers to schedule me an appointment yet. I have been receiving mental health care from the VA for nearly 8 years!
Ive been begging for help for years from reps /comp drs, been ignored every time they have a excuse list to cover their incompetence ,errors laziness out right incompetence thats miles long!!!!!!!!! their Motto is DELAY THEM TILL THEY DIE
See my comments under Veterans Suicide…and realize the constant Harassment I have been receiving from the VA has INCREASED my STRESS (PTSD) by 100!! I had to move to a Rural Area to easy my Stress Levels, only to discover that there is no Law Enforcement in Chippewa County, Wisconsin. The VA in Wisconsin harassed me for & year about my Property Tax Rebate as a Disabled Veteran, it states 5 years after outsiders move to Wisconsin.
I have a neighbor who tries to take advantage of my PTSD by piling trash along my property live, shooting guns to rattle me and disturbing the peace all weekend and in the evenings. When I complain, the Sheriff and the Town Council tell me they CAN NOT or WILL NOT enforce laws here.
I am denied my legal rights!!
I know why Our Brothers and Sisters are ending their lives. THE VA DOES NOT CARE and they prove it every day. We wait up to 2 months for pain meds. The excuse. The Dr has too many patients to sign all prescriptions We are doing the best we can. That is BS. We call and No one answers the phone. I spent 18 hours in 3 days trying to get my meds refilled I had to call my Congress Woman’s office to get it done Our Regular Dr visits have gone from every 3 months to every 7 months. Your staffing problems are YOUR problems not ours but we pay for it with substandard care. The Nurses are great and they care but you can not keep Doctors. I have had 12 in the last 7 years. I have only laid eyes on 1 Doctor in all this time.
Suggestion. Sell all the BA facilities Fire all the employees and save Billions while giving us a Card allowing us to go to our Home town Doctor. You will save tons of money and we will finally get Healthcare that we Deserve. Many of us were wounded in Combat. We did our part and our ills are combat related. Agent Orange is the big Demon.
Our country let us down in Viet Nam and is still doing so with the VA and their so called Health Care.
That is why 23-26 Vets are killing them selves per day. Frustration from day after day being denied adequate Healthcare and poor management of the VA system. Shame on you.
I forgot to add for accuracy’s sake that a referral that was put in for me last November was canceled without me being told. When I called the Patient Advocate the appointment was rescheduled for this coming October.
That is considered an appropriate waiting time? Eleven months?
The appointments need to be scheduled through your PCP? The first appointment available there is in mid-June. How long do you expect Vets to “hold on”?????
Timely healthcare access continues to be a barrier for Veteran’s health, especially mental health matters. In the near 10-year span between 2005 and 2014, Vets who received VA provided mental healthcare services increased by 71%, almost doubling the number of mental health visits from 2005 (Senate veterans’ affairs committee hearing, 2015). In October 2015, there were new guidelines released regarding service access and relative wait times; since then, the wait time for full evaluation has averaged about 26 days, with acute care provision provided within 24 hours of their initial request for a visit (Senate veterans’ affairs committee hearing, 2015). Vets in need may be seen through ER or by their health care provider for immediate needs, and then they return for a full intake visit with a mental health provider within the month.
These guidelines continue to be modified, in an attempt to increase access and communication. There are now same day services when medically necessary, and an app called My VA Access to assist in appointment making (VA plan calls for same-day access to health care services, 2016). Same day appointments reduce ER visits and often bode well as far as continuity of care with the PCP. Collaborative care between the PCP and mental health providers would reduce ER visits for mental health concerns (Yoon, Cordasco, Chow, & Rubenstein, 2015). This requires an improved referral system and improved coordination of care between the providers. The mental health of our veterans is spoken of frequently and seriously. Government incentives should be in place to help recruit providers to address the growing need in mental health and suicide prevention. Patients and their loved ones must stay hopeful and continue to seek care so that our Vets are not lost or left behind.
The Federal Government has provided many services and incentives for veterans returning from war or service. They include health care, education, job training, home loans, and disability compensation (Gade, 2019). These services are beneficial for veterans and are well intended, but they do little to deal with underlying issues such as post-traumatic stress disorder, depression, and feelings of worthlessness. Recently Congress and President Trump have passed Mission Act of 2018 to improve the VA’s ability to deliver quality and timely care to Veterans (U.S. Department of Veterans Affairs, 2019). This bill has promised easy and reliable access for Veterans to received same day services through the VA and community care programs (VA Mission Act of 2018). The opportunity for Veterans and their families to receive timely care will be an improvement compared to previous systems. However, we need to encourage State and National Governments to use a portion of the $200 billion budgeted for the VA to implement policies that can also offer promotion of individual value, health, and wellbeing. The future efforts of the VA must not only increase access and quality of healthcare, but they must promote productive lives independent of disability, increase post-military work opportunities while addressing mental health issues. Including these topics in future bills will improve mental health concerns, will reduce homelessness, improve adaptation to civilian life, and prevent suicide. I feel the VA has been making attempts to improve their quality of care after being ridiculed for years. However, mental health access, patient-centered care, and promotion of self-worth have been lagging.
Bull C***. In Austin Texas the wait to get help is six to eight weeks for a teleconference. We recently had a veteran shoot himself in the restroom of our VA facility out of frustration. Nothing is even being said or done. How many more veterans will have to kill themselves in frustration before they decide to take this seriously? With VA it’s not lack of funding, it’s lack of will.
Bull C***. In Austin Texas the wait to get help is six to eight weeks for a teleconference. We recently had a veteran shoot himself in the restroom of our VA facility out of frustration. Nothing is even being said or done. How many more veterans will have to kill themselves in frustration before they decide to take this seriously? With VA it’s not lack of funding, it’s lack of will.
Five years ago, I thought people who said “the VA wants us dead” were crazy. I thought it was a small percent of the veteran community overreacting and being hysterical. Today, I KNOW the VA wants us dead. The first time I went to Baypines VA, a Vietnam Veteran took his life in the parking lot after being turned away from the ER. He went to the ER in emotional/mental crisis asking for help and was turned away, was told the ER wasn’t the appropriate place for him to seek help and he needed to make an appointment with MH. He went home, retrieved his weapon and returned to the parking lot to end the suffering he could no longer bear. They absolutely want us dead, they provide appropriate MHC for veterans suffering PTSD etc. They sure as hell don’t want to continue financially “compensating” us, when a Vet dies the VA can save up to 3K per month. Over 20 vets a day lost to suicide, horrifically the VA sees that as a financial victory for them.